SHOULDER INSTABILITY
The shoulder joint is a shallow ball and socket joint which allows for great movement but comes at the risk of shoulder instability. The joint capsule, ligaments and rotator cuff muscles are crucial in maintaining the stability but need to be elastic and flexible to allow movement to occur. The socket is made deeper by a rim of fibrocartilage (labrum).
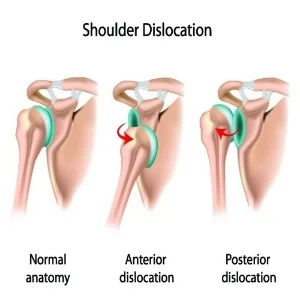
A shoulder dislocation occurs when the ball (humerus) comes out of the socket (glenoid). This may be partial (subluxation) or full (dislocation). After the first episode, it is likely that the labrum and ligaments will be torn, putting the shoulder at high risk of recurrent episodes of instability. This is especially true for patients under the age of 25 years.
Recurrent shoulder instability following a traumatic shoulder dislocation can be effectively treated by repairing the torn labrum and ligaments. This is most commonly done using keyhole (arthroscopic) surgery and, when using modern techniques, is associated with a high rate of success. The labrum is reattached to the edge of the socket and the ligaments are tightened. This is done using suture anchors inserted into the edge of the socket (glenoid).
If you have had several episodes, the bone on the front of the socket can be damaged. This means that keyhole surgery is less effective and open surgery is preferred when there is damage to the bone.
Labral Tear (Bankart lesion)
Bankart Repair
Recovery following surgery usually involves being in a sling for 6 weeks. Most people can drive a car after 6 to 8 weeks. Rehabilitation guidelines to share with your physiotherapist are provided following the surgery. Physiotherapy usually starts after 6 weeks following surgery. Return sport is usually possible at 6 months.
Risks of surgery include infection, stiffness, ongoing pain and instability, re-tear of the labral repair, and very rarely, nerve injury. Antibiotics are given at the time of surgery to minimize the risk of infection. Despite this, infection of the wounds can occur. This is usually easily treated with antibiotics. However, sometimes the infection gets into the joint, which is a serious complication and requires re-admission to hospital, additional surgery and intravenous antibiotics.
Atraumatic shoulder instability occurs less commonly. This is where the shoulder dislocates with minimal effort and these patients are often described as “loose jointed”. Unlike traumatic shoulder instability, there usually isn’t a labral tear and most patients are treated with physiotherapy.